There are a number of things that may contribute to or cause gastroparesis. In the majority of people with gastroparesis, the cause is unknown and is termed “idiopathic.” This is the most common subset of gastroparesis. The term idiopathic simply means that there is no known cause of the disease. An average of 30% to 50% of patients with gastroparesis have a diagnosis of idiopathic gastroparesis. Some people with idiopathic gastroparesis report symptoms following a virus infection (post-infectious or post-viral gastroparesis). Although there are many potential causes of idiopathic Gastroparesis, more research is needed to verify if these are true causes or risk factors for developing GP.
Other possible causes of gastroparesis include:
- Diabetes
- Surgeries
- Medications
- Other illnesses
- Cellular changes
Diabetes
Gastroparesis may occur as a complication of other conditions. Long-standing diabetes is the most common known cause of gastroparesis, although only a small percentage of people with diabetes develop gastroparesis.
Diabetes mellitus is a disorder in which the body does not produce enough or respond normally to insulin. Insulin is a hormone released by the pancreas that regulates blood sugar. This condition causes higher than normal levels of sugar in the blood. Diabetic gastroparesis occurs when slow emptying of the stomach occurs in people with diabetes.
About 25% of gastroparesis patients are diagnosed with diabetic gastroparesis. This can affect people with either type 1 or type 2 diabetes. In patients who develop diabetic GP, symptoms usually continue, even if sugar levels become controlled. Diabetic GP occurs in a similar way as diabetic neuropathy, such as what commonly occurs in the feet of those with diabetes. Nerve damage occurs over time as a result of uncontrolled sugar levels in the body. In diabetic foot neuropathy this impacts the long nerves that extend to the feet. For diabetic GP, this nerve damage occurs in the nerves that go into and surround the stomach.
Viral Infections
In many people, viral infections are a cause. These are called viral gastroenteritis, which are viruses affecting the GI system. This can be due to any viruses that cause GI symptoms- even COVID-19. Others are norovirus and rotavirus infections which commonly affect children. Some people who develop GP from viruses may feel relief of symptoms months or years later.
Surgeries
GP can occur when surgery changes the stomach. This can be through damage to nerves or the formation of scar tissue damage to the stomach. The vagus nerve, if damaged, is often believed to be the cause in patients who suffer from GP symptoms. The vagus nerve originates in the brain and extends to control major body organs such as the heart, lungs, upper GI tract, and other organs in the chest and abdomen.
Surgeries that cause some cases of GP include:
- Nissen fundoplication– This is a surgery for Gastroesophageal Reflux Disease (GERD) or hiatal hernia.
- Cholecystectomy– This surgery refers to removing the gallbladder usually due to right upper abdominal pain or stones called gallstones that could accumulate in the gallbladder and cause infection or blockage.
Medications
Less frequently, gastroparesis is seen to occur after the use of certain medications. Some medications can impair motility. Examples include:
- narcotic pain relievers,
- anticholinergic/antispasmodic agents,
- calcium channel blockers,
- some antidepressants, and
- some medications for diabetes.
Other Illnesses
Other causes of GP are neurologic. Neurological conditions such as Parkinson’s Disease can impact GP by affecting the nerves that supply the stomach. Multiple sclerosis (MS) is another neurologic condition where patients often develop GP. Connective tissue diseases like lupus and scleroderma can also lead to GP. This due to smooth muscles in the stomach weakening as a result of the disease process. These conditions cause smooth muscles to break down in the body including the GI tract. Smooth muscles are located throughout the body and contract, or put pressure on, internal organs and blood vessels.
Cellular Changes
Much remains to be learned about what causes gastroparesis. In both idiopathic and diabetic gastroparesis a great deal of interest is being paid to changes in the cells which help control muscular contractions (motility) in the stomach. These are known as the interstitial cells of Cajal (ICCs). These cells probably represent the essential pacemakers of the entire gastrointestinal (GI) tract. In addition to ICCs, scientists are looking at changes in the structure and the number of nerve cells and immune cells as possible contributors to the disease process in gastroparesis.
Potential Causes for Gastroparesis Reported by Patients
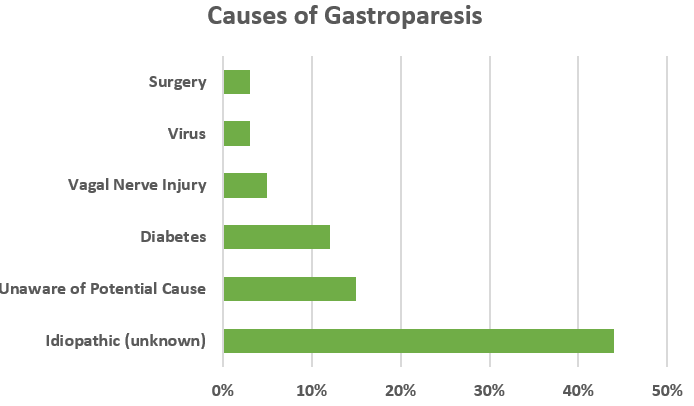
Respondents (1,423 adults) in the 2016 Gastroparesis in the Community Research Survey were asked, did the doctor who diagnosed you indicate a potential cause of your gastroparesis. Idiopathic gastroparesis (unknown cause) was most frequently suggested:
Adapted from IFFGD Publication: Gastroparesis Overview by: Baharak Moshiree MD MSc, Mackenzie Jarvis PA-C, DMs, Atrium Health, Wake Forest, Digestive Health-Morehead Medical Plaza; Marissa Lombardi, International Foundation for Gastrointestinal Disorders, Mt. Pleasant, SC










